Researchers from the University Hospital of Würzburg have discovered a new regulatory mechanism of blood clotting that could have great clinical potential. In hemostasis, blood platelets attach to wound edges to form a plug, while blood coagulation leads to the formation of long fibrin fibers that seal the wound. However, excess fibrin can lead to thrombosis and vascular occlusions, making regulation of fibrin formation essential. The researchers identified glycoprotein V (GPV) as a new switching point that regulates both hemostasis and thrombosis. GPV, which is expressed on the surface of blood platelets, controls the activity of the enzyme thrombin that is responsible for fibrin formation. In another approach, the research group generated antibodies against GPV that prevent thrombin-mediated cleavage of GPV, increasing thrombin activity and resulting in increased fibrin formation. The researchers’ idea was to use these antibodies to increase fibrin formation in the context of impaired hemostasis. The new antibody developed by the research group was able to restore hemostasis under conditions where it is not possible otherwise in an experimental model of hemostasis, indicating that it enhances thrombin-dependent fibrin formation.
A new regulatory mechanism of blood clotting has been discovered by researchers from the University Hospital of Würzburg in an international project. Hemostasis, the process of stopping bleeding and sealing wounds, involves blood platelets forming a plug and blood coagulation leading to the formation of long fibrin fibers that seal the wound. However, excess fibrin can lead to thrombosis and vascular occlusions, making regulation of fibrin formation essential.
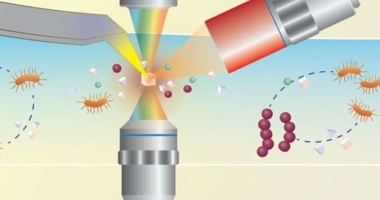
In the study, the researchers identified glycoprotein V (GPV) as a new switching point that regulates both hemostasis and thrombosis. GPV, which is expressed on the surface of blood platelets, controls the activity of the enzyme thrombin that is responsible for fibrin formation. Thrombin is an essential enzyme in blood clotting, and its activity must be precisely controlled. The surface receptor GPV is cleaved by thrombin during platelet activation, releasing it as a soluble form.
The physiological function of this receptor was previously unknown, but the researchers found that thrombin-mediated cleavage of GPV limits fibrin formation. Soluble GPV, remaining bound to thrombin, alters the activity of thrombin so that it can form less fibrin.
The researchers propose new therapeutic approaches based on this discovery, and the results have been published in the journal Nature Cardiovascular Research. Professor Bernhard Nieswandt, head of the Institute of Experimental Biomedicine I and member of the board of the Rudolf Virchow Center, said that the findings will change textbook knowledge, as this is the first time a new switching point has been uncovered that regulates both hemostasis and thrombosis.
A treatment using soluble GPV was also tested in an experimental mouse model of thrombosis formation, which showed that it prevents the formation of a vessel-occluding thrombus. The discovery of this new regulatory mechanism of fibrin formation and its potential clinical applications could have a significant impact on future treatments for thrombosis and other related conditions.
Soluble GPV has been shown to prevent the formation of vaso-occlusive thrombi and provide significant protection against experimental stroke and associated brain damage in experimental thrombosis models. Professor Bernhard Nieswandt believes that these findings will change textbook knowledge and expresses his gratitude to all participating scientists from the RVZ and the University Hospital Würzburg, who received support from colleagues in Mainz, Maastricht, and the USA.
In another approach, the research group generated antibodies against GPV that prevent thrombin-mediated cleavage of GPV. These antibodies increase thrombin activity, resulting in increased fibrin formation. The researchers’ idea was to use these antibodies in the context of impaired hemostasis to increase fibrin formation. Dr Sarah Beck, first author of the study and scientist at the Würzburg Institute for Experimental Biomedicine, notes that the treatment with platelet aggregation inhibitors such as clopidogrel impairs platelet function and leads to reduced platelet count or impaired function, in addition to genetic causes.
The new antibody developed by the research group was able to restore hemostasis under conditions where it is not possible otherwise in an experimental model of hemostasis, indicating that it enhances thrombin-dependent fibrin formation. According to Dr Beck, anti-GPV treatment has great clinical potential and will be further investigated in the future. The study was conducted by researchers from the RVZ and the University Hospital of Würzburg, with support from colleagues in Mainz, Maastricht, and the USA. A disclaimer states that AAAS and EurekAlert! are not responsible for the accuracy of news releases or the use of any information through the EurekAlert system.
Don’t miss interesting posts on Famousbio