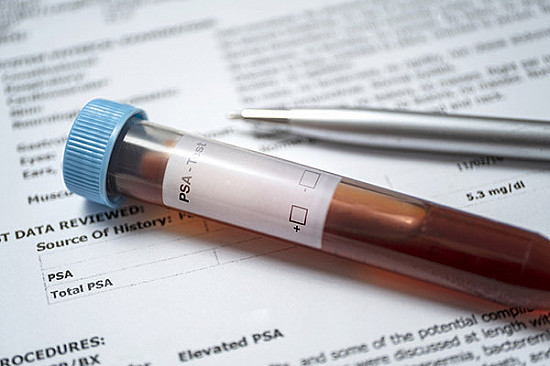
As the transgender population grows, it is important to understand their health outcomes and how best to care for them. Hormone therapy given to transgender women reduces the overall risk of prostate cancer, but the interpretation of prostate cancer rates is limited by the barriers to care they experience. Furthermore, there are no guideline recommendations for prostate-specific antigen (PSA) screening in the transgender population. The PSA cutoff of 4 nanograms per milliliter (ng/mL) of blood is specific to cisgender men, so researchers propose capping the limit for what’s considered normal in transgender women at 1.0 ng/mL. Doctors must take extra care when interpreting PSA values in transgender women. Further research is needed to better understand the relationship between hormone therapy and prostate cancer in transgender women.
Prostate Cancer in Transgender Women: A Review of Current Knowledge
As the transgender population grows, it has important implications for public health. Hormone treatment given to transgender women reduces the overall risk of prostate cancer, according to a recent paper.
The number of transgender people is on the rise. In the US alone, 1.3% of people between the ages of 18 and 24 identify as transgender, compared to 0.55% of older adults. This trend has raised concerns about the risk of prostate cancer in transgender women.
Doctors generally leave the prostate gland in place when initiating hormone therapy to induce female sex characteristics in transitioning individuals. This process, called gender-affirming hormonal therapy (GAHT), relies on medications and surgery to block testosterone, the male sex hormone. GAHT lowers overall risks for prostate cancer since the disease is fueled by testosterone. However, transgender women can still develop prostate cancer in ways that are not yet fully understood.
To gain better insights into the incidence and screening rates of prostate cancer among transgender women, Dr. Farnoosh Nik-Ahd, a urologist at the University of California, San Francisco, and her colleagues performed a comprehensive review of the literature. They found that the prevalence of GAHT in the transgender population is still unknown. Studies estimate the figure to be around one in every 12,000 to 13,000 people, but the authors claim that this is likely an underestimate, and it’s not broken out by sex.
Similarly, little is known about the impact of GAHT on the likelihood of developing prostate cancer. The team reported that prostate cancer rates appear to be lower among transgender women than they are among cisgender men. For example, a study found only one case of prostate cancer among 2,306 transgender women receiving routine healthcare at a clinic in Amsterdam, Holland, between 1975 and 2006. Another study detected six cases of prostate cancer among 2,281 transgender women over 17 years, which again is less than the comparable rate among cisgender men.
The authors note that “More individuals are openly identifying as transgender, particularly as advances are made in reducing the discrimination and marginalization that this group has faced. Thus, it’s important to understand their health outcomes and how best to care for this population.”
It is clear that more research is needed to fully understand the relationship between hormone therapy and prostate cancer in transgender women. Nonetheless, this paper provides a valuable review of current knowledge and highlights areas where further study is necessary.
Prostate Cancer and Transgender Women: Overcoming Barriers to Care
The prevalence of transgender individuals is steadily increasing, but the risks of prostate cancer in transgender women remain poorly understood. While hormone therapy can lower the overall risk of prostate cancer, transgender women can still develop the disease. A recent paper highlights the need for further research on prostate cancer incidence and screening rates among transgender women, as well as the barriers to care that they face.
Barriers to Care for Transgender Women
Transgender women often experience barriers to care due to financial hardship and fear of mistreatment. As a result, many avoid seeking medical help, which can limit the interpretation of prostate cancer rates among this population. Additionally, some scientists have raised concerns that estrogen given during gender-affirming hormonal therapy (GAHT) may contribute to prostate cancer development over long durations, but further evidence is needed.
PSA Screening Recommendations for Transgender Women
The lack of guideline recommendations for prostate-specific antigen (PSA) screening in the transgender population is a significant concern. None of the available guidelines worldwide mention transgender women, and the PSA cutoff of 4 nanograms per milliliter (ng/mL) of blood is specific to cisgender men. Since PSA levels plummet in people taking GAHT, the researchers propose capping the limit for what’s considered normal in transgender women at 1.0 ng/mL. They also recommend that people meeting age criteria for PSA screening get tested before starting on GAHT to establish a baseline value.
Education for Primary Care Doctors and the Transgender Community
Doctors must take extra care when interpreting PSA values in transgender women, just as they do with other common drugs that alter PSA values in cisgender men. Broader education on this topic is necessary for primary care doctors as well as the transgender community. The lack of data on GAHT use in a study on survival among transgender women with prostate cancer is also concerning. Future research should aim to understand baseline PSA values for those on GAHT and to navigate some of the psychosocial barriers around PSA screening to avoid stigmatizing transgender patients.
In conclusion, the interpretation of prostate cancer rates among transgender women is limited by the barriers to care that they face. The lack of guideline recommendations for PSA screening in this population is a significant concern, and doctors must take extra care when interpreting PSA values. Broader education on this topic is necessary for primary care doctors as well as the transgender community. Further research is needed to better understand the relationship between GAHT and prostate cancer in transgender women.
Don’t miss interesting posts on Famousbio