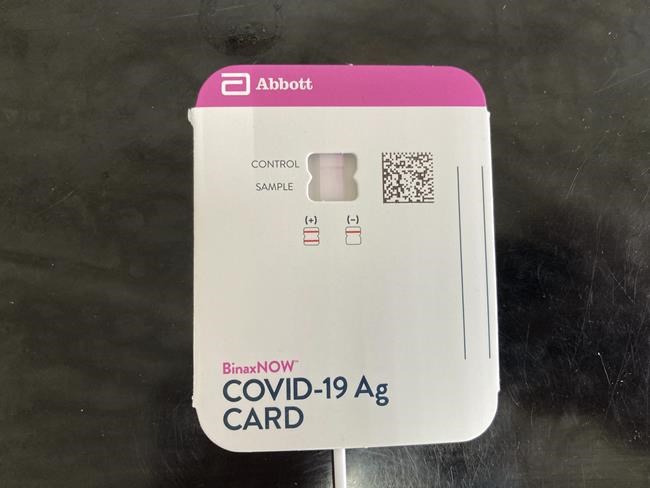
LOWRY CITY, Mo. (AP) — At Truman Lake Manor in rural Missouri, every day begins the same way for every employee who walks through the doors of the nursing home — with a nasal swab, a squirt of test solution and a brief wait whether a thin red line appears, indicating a positive COVID-19 case.
Only the healthy are allowed in to ensure virus-free residents.
Despite these precautions, a coronavirus outbreak swept through the facility late last year. An inspector then cited it for violating the federal government’s COVID-19 vaccination requirement for healthcare facilities.
Truman Lake Manor is one of about 750 nursing homes and 110 hospitals nationwide charged with violating federal staff vaccination requirements last year, according to an Associated Press analysis of data from the Centers for Medicare & Medicaid Services. Most received a bureaucratic push to do better – although some care homes also received fines, particularly if they had several other problems.
A year after its nationwide enforcement began on February 20, 2022, mandatory vaccination, which will affect an estimated 10 million healthcare workers, is the last remaining major mandate from President Joe Biden’s sweeping attempt to increase national immunization rates. Similar requirements for large employers, members of the military and federal contractors have all been rescinded, lifted or partially blocked.
The public health vaccination mandate is set to run until November 2024. However, some claim it is time to stop now, citing less severe COVID-19 cases, healthcare workforce shortages and the imminent expiry of a national public health emergency on May 11 since January 2020.
“Their regulations are making them harder to look after – not easier,” said Tim Corbin, Truman Lake Manor’s administrator, who also serves as a nurse, adding that “mandates must end.”
CMS said in a statement to the AP that “requiring staff to be fully vaccinated was a critical step in the response to the pandemic” and “saved Americans from countless infections, hospitalizations and death.”
The policy requires workers, contractors, and volunteers at facilities receiving Medicare or Medicaid payments to receive the full primary dose of an original COVID-19 vaccine, with exceptions for medical or religious reasons. Although nursing homes can be fined for violators, CMS has generally given violating facilities additional time to update their policies and comply with regulations.
The Republican-led US House of Representatives recently passed legislation that would halt the mandate, but the law is unlikely to pass in the Democrat-led Senate.
Meanwhile, the request continues with mixed results and – in some cases – widespread exceptions.
When a state inspector visited Truman Lake Manor in December, a coronavirus outbreak in recent weeks had infected 26 of the 60 residents and about a quarter of the staff. Corbin said the outbreak originated from an unvaccinated employee on a religious exemption who tested negative for COVID-19 and wore a mask before working shifts. The employee was not feeling well and tested positive after arriving home.
The inspector found that more than 40% of staff had been granted religious exemptions from vaccination. However, the federal Centers for Medicare & Medicaid Services do not review the rationale for such exceptions. The reason the facility was cited for a vaccine shortage was that three staff members had not received their second dose of the vaccine and no exemption was on record. After the subpoena, they were each given a second chance, and regulators admitted to the corrections in January.
It’s difficult to find workers willing to get vaccinated, Corbin said, because many local residents continue to oppose the vaccine or doubt its effectiveness. Just 42% of adults in St. Clair County are vaccinated against COVID-19 — a rate barely half the national average.
At a facility in Greenwood, South Carolina, the vaccination order caused a drain of nursing staff that took a while to replenish.
According to the American Health Care Association, which represents long-term care facilities, labor shortages are prompting more than half of nursing homes across the country to limit occupancy of residents. Although most other healthcare sectors have recovered, nursing home employment in 2022 fell 13% from pre-pandemic levels, reaching a low not seen since the 1990s.
LeadingAge, a coalition of nonprofit nursing homes and other aging service providers, originally supported the mandate and still promotes vaccination. But it is now said that a federal requirement is no longer needed.
Although the number of deaths has declined significantly since its peak in January 2021, older adults and those with underlying health conditions remain more vulnerable to severe cases of COVID-19. Because of this, some medical professionals believe the vaccination mandate should continue in nursing homes and hospitals.
“This is an important requirement,” said Dr. Georges Benjamin, executive director of the American Public Health Association. “It not only protects the medical staff themselves, but also the patients.”
According to the AP analysis, about 5% of the more than 15,000 nursing homes serving Medicare or Medicaid patients nationwide have been charged with COVID-19 immunization violations and about 2% of the 4,900 hospitals. However, these citations were not evenly distributed across the states and occurred less frequently in the second half of 2022.
24 states did not name hospitals for COVID-19 vaccination violations.
Kansas, Florida and Texas each declined to search for vaccination violations, instead leaving that process to CMS, which hired contractors. As a result, CMS said Texas was docked more than $2.5 million in federal funding, Florida more than $1.2 million, and Kansas nearly $350,000.
Kansas Gov. Laura Kelly, a Democrat facing re-election in a Republican state, said last year that the immunization mandate violated state law and could exacerbate labor shortages.
Nationwide, the number of nursing homes cited for immunization violations fell noticeably after CMS last June stopped requiring state inspectors to review compliance when responding to complaints about unrelated allegations such as patient neglect. When making the change, CMS relied on extensive compliance with the vaccination requirement.
__
Harjai reported from Los Angeles and is a corps member of the Associated Press/Report for America Statehouse News Initiative. Report for America is a nonprofit national service program that places journalists in local newsrooms to cover undercover topics.
David A. Lieb and Kavish Harjai, The Associated Press
Don’t miss interesting posts on Famousbio