“Stanford Scientists Create Synthetic Molecule to Target and Destroy Cancerous Tumors”
[Feb. 7, 2023: Krista Conger, Stanford Medicine]
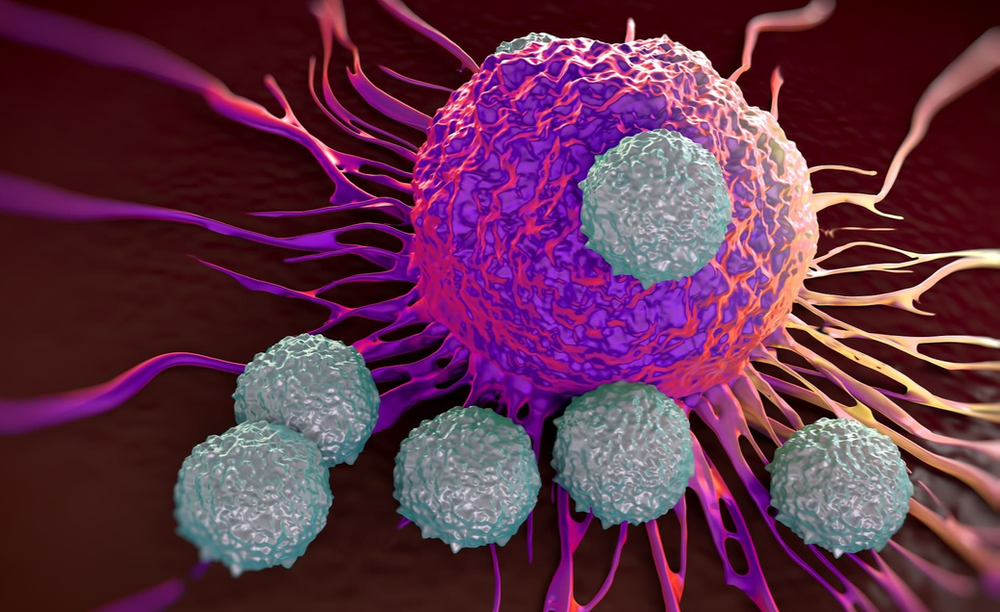
Activating the immune system at the site of a tumor can recruit and stimulate immune cells to destroy tumor cells. (PHOTO CREDIT: Creative Commons)
Activating the immune system at the site of a tumor can recruit and stimulate immune cells to destroy tumor cells. One strategy is to inject immune-stimulating molecules directly into the tumor, but this method can be challenging for hard-to-reach cancers.
Now Stanford researchers have developed a new synthetic molecule that combines a tumor-targeting agent with another molecule that triggers immune activation. This tumor-targeted immunotherapy can be given intravenously and delivered to one or more tumor sites in the body, where it recruits immune cells to fight the cancer.
Three doses of this new immunotherapy prolonged the survival of six out of nine laboratory mice with aggressive triple-negative breast cancer. Of the six, three appeared cured of their cancer during the month-long study. A single dose of this molecule induced complete tumor regression in five out of ten mice. The synthetic molecule showed similar results in a mouse model of pancreatic cancer.
“We essentially cured some animals with just a few injections,” said Jennifer Cochran, PhD, the Shriram chair of the Department of Bioengineering. “It was pretty amazing. When we looked inside the tumors, we saw that they changed from a highly immunosuppressive microenvironment to one full of activated B and T cells – similar to when the immunostimulatory molecule is injected directly into the tumor. So we’re getting intratumoral injection results, but with an IV delivery.”
similar posts
An article describing the study will be published online in Cell Chemical Biology. Cochran shares senior authorship with Carolyn Bertozzi, PhD, the Baker Family Director of Stanford ChEM-H, Anne T. and Robert M. Bass Professor in the School of Humanities and Sciences and Professor of Chemistry; and Ronald Levy, MD, Robert K. and Helen K. Summy Professor at the School of Medicine. The lead authors are graduate student Caitlyn Miller and medical professor Idit Sagiv-Barfi, PhD.
Building on previous research
The treatment builds on an earlier study co-authored by Levy and Sagiv-Barfi in which the same immune-activating agent and a different one were injected directly into the tumor site.
This study showed that the combination could eradicate both tumors in mice and distant metastases. It also blocked the development of tumors in mice that had been genetically engineered to spontaneously develop breast tumors. This finding started an ongoing clinical trial in people with non-Hodgkin lymphoma.
“The surprising result of the new research was that the shaping of the tumor microenvironment by this intravenously administered molecule was identical to that achieved by direct injection of immunostimulatory drugs into the tumor,” Levy said. “This is a great advantage because it is no longer necessary to have an easily or safely injectable tumor site.”
Systemic dosing of PIP-CpG is more effective than free CpG in mouse cancer models. (CREDIT: Stanford Medicine)
Much research is still needed to determine if and when the molecule, dubbed PIP-CpG, will be ready for human testing. However, because the tumor-targeting part of the molecule – PIP – recognizes specific proteins called integrins, which are found at high levels on the surface of many types of cancer cells, the research suggests the future possibility of a standard treatment for patients with a variety of cancer types .
“PIP is a really versatile tumor-targeting agent because it can localize to so many different types of tumors,” Miller said. “Furthermore, the same molecule is biologically active in mice, non-human primates and humans.”
Ronald Levy (left) and Idit Sagiv-Barfi led work on a potential cancer treatment that involves direct injection of two immune-stimulating agents into solid tumors. (PHOTO CREDIT: Steve Fish)
With professor emeritus of developmental biology Matthew Scott, PhD, and late professor and chair of radiology Sanjiv “Sam” Gambhir, MD, PhD, Cochran has the ability to seek out and bind to PIP developed in Cochran’s lab , studies integrins on the surface of cancer cells. By coupling these molecules to probes that can be visualized by near-infrared imaging or positron emission tomography, researchers can track the location of hard-to-see cancers in the body.
In other work at the Cochran lab, researchers, in collaboration with the Stanford ChEM-H Medicinal Chemistry Knowledge Center, have created conjugates that seek out cancer cells and deliver a cargo of chemotherapy toxins to the tumor.
“These integrin targeting molecules act like guided missiles,” Cochran said. “They can deliver toxic drugs or imaging agents. Now we’re using them to deliver a signal that triggers the immune cells to fight the tumor.” That signal, CpG, mimics a DNA pattern that’s common in bacteria and viruses but rare in vertebrates.
Certain types of tumors, including some breast cancers, use natural regulatory pathways to suppress the activity of cancer-killing immune cells that have infiltrated the tumor – rendering them immunologically “cold.”
Miller and Sagiv-Barfi found that PIP-CpG treatment turned these breast cancer tumors in the mice into “hot” tumors teeming with activated T and B cells. The treatment also reduced the prevalence of another type of immunosuppressive cells called myeloid suppressor cells in the tumor.
The researchers also showed that the treatment can also attack multiple tumors in an animal.
“After more than 10 years of work on PIP, it is rewarding to see this convergence of expertise from Stanford-area laboratories that has enabled us to develop a promising new cancer treatment strategy,” said Cochran.
Jennifer Cochran & fourth year graduate student. (CREDIT: Stanford Medical)
Researchers are now studying the treatment in other types of cancer and in combination with other immunotherapies.
Other Stanford authors on the study include Instructor Patrick Neuhofer, PhD; senior research scientist Debra Czerwinski; and Professor of Biochemistry Steven Artandi, MD, PhD.
For more scientific news, visit our New Innovations section at The lighter side of the news.
Note: Materials provided above by Stanford Medicine. Content can be edited for style and length.
Like those kind of feel-good stories? get that Brighter Side of News newsletter.
Source: www.thebrighterside.news
Don’t miss interesting posts on Famousbio