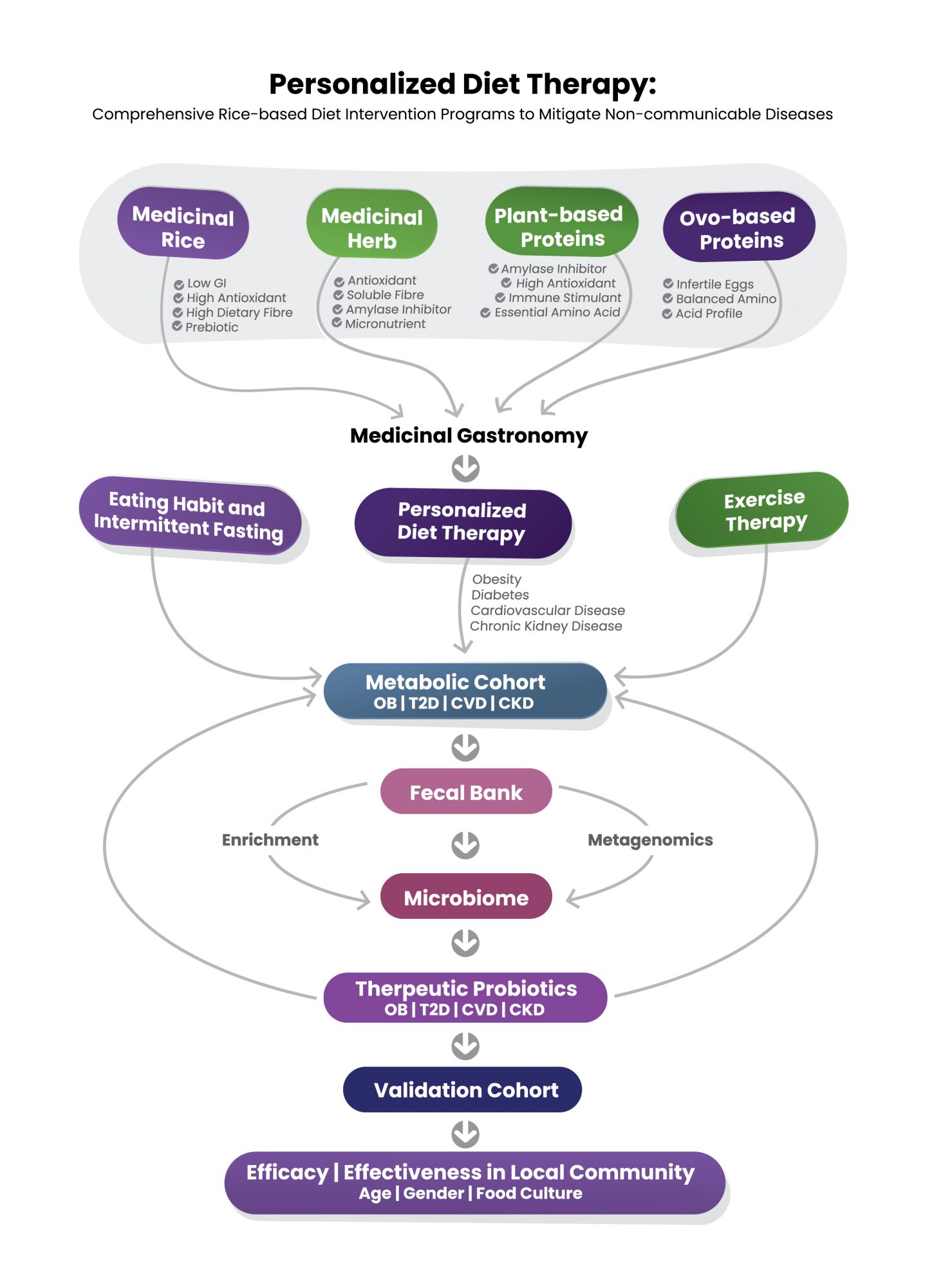
Thai researchers have developed personalised diets to prevent non-communicable diseases (NCDs) such as obesity, diabetes, and cardiovascular disease in the country’s ageing population. The researchers used 3G rice, a mixture of intermediate to low glycemic index rice varieties, in the diets. The researchers also designed 29 meal plans based on medical restrictions, food allergies, food restrictions, gender, age, and occupation, and included exercise therapy as part of the diet intervention program. Stools collected from participants were analysed for gut microbiota, leading to the identification of 90 microbial isolates from patients with NCDs. The isolated gut microbiota contained different ratios of hemolytic bacteria, depending on whether the patient had obesity or type-2 diabetes. This ongoing project has been financially supported by the National Research Council of Thailand.
Professor Apichart Vanavichit has conducted research on personalized diet intervention and therapy for Thailand’s ageing population to prevent non-communicable diseases (NCDs) like obesity, type-2 diabetes, and cardiovascular disease. With an increasing elderly population, it is predicted that the prevalence of NCDs will also rise.
The incidence of type-2 diabetes has seen a significant increase from 6.5% in 2015 to an estimated 10.7% in 2030, with the highest prevalence expected among the elderly population (72%). The burden of NCDs is high in developing countries and is most common among the poor elderly whose life depends on their children. To slow down the prevalence of future NCDs, lower glycemic index meals and lifestyle changes through diet intervention programs are viable solutions.
The research established a metabolic cohort (MBC) consisting of 146 participants, including adult males between 37 and 60 years old, who were screened for biomarkers, gut microbiota, fat mass, MRI-scanned visceral fat, and hepatic fat. The MBC was then divided into obesity, type-2 diabetes, cardiovascular disease, and chronic kidney diseases groups to understand the impact of redesigned meals on NCDs among adults.
The MBC underwent three months of diet intervention and exercise programs, while the no-intervention group was used as a control. Biomarkers, body weight, body mass index, gut microbiota, fat mass, visceral fat, hepatic fat, and daily food records were tracked for three and twelve months at Siriraj Hospital, Bangkok, following the exercise and diet intervention programs compared to the non-intervention group.
The study developed a low glycemic index rice mixture, as shown in Figure 2. Redesigned rice-based local meals with this mixture were used to monitor the benefits of diet intervention in the MBC. The study demonstrated that personalized diet intervention and lifestyle changes can reduce the prevalence of NCDs among the ageing population of Thailand.
Overall, the study recommends developing personalized diet intervention programs for the elderly population to prevent the future prevalence of NCDs like obesity, type-2 diabetes, and cardiovascular disease in Thailand.
Personalized diet recipes were developed from popular local dishes to meet medical restrictions, body weight, body mass index, food allergies, food restrictions, gender, age, and occupation. With rice contributing over 50% of the energy in daily rice-based meals among Thais, a new mixture of intermediate to low glycemic index rice varieties called 3G rice was developed to control total daily energy targets of personalized diet intervention plans.
The study successfully designed 29 recipes to meet personalized targeted total daily energy, ranging from 1000 to 2000 kcal. Medical restrictions were laid out by doctors and dietitians to limit sugar, sodium, fat, trans-fat, saturated fatty acids, and protein. Meals contained carbohydrates, protein, and fat equal to 45-50%, 20-30%, and 20-30%, respectively. Additionally, Na, Ca, K, and P were controlled at <2,000 mg, <1,200 mg, <2,800-4,500 mg, and <800 mg, respectively.
To avoid repetitiveness, different menus within each category of medical restriction were rotated weekly by participants. Participants received 3G mixed rice and well-designed meals, freshly made daily for early-morning home delivery, for three months. Daily food consumption and exercise practices were recorded throughout the study. Participants were satisfied with the taste and nutritional quality of 3G rice-based meals.
The exercise therapy program, Pliability, was designed for elderly patients to optimize muscle strength and flexibility by walking for at least 6,000-7,000 steps daily with aerobic exercise programs. Participants were grouped based on their BMIs into three degrees of obesity, OB1, OB2, and OB3, for BMI 23-24.9, BMI 25-29.90, and BMI >30, respectively.
All participants were recommended 20-30 minutes of aerobic exercise and pliable programs designed for each OB group. The exercise therapy was monitored daily via a smartwatch for 1, 3, 6, and 12 months. The outcomes varied by the OB groups. The number of days required to reduce BMI to 23, the regular scale, was monitored for each group. For OB1, 70% of participants reached the normal BMI by 45 days, while OB3 required 180 days. In the worst case, 20% of participants needed 300 days to achieve a BMI of 23.
Overall, the study showed that personalized diet intervention and lifestyle changes can reduce the prevalence of non-communicable diseases like obesity, type-2 diabetes, and cardiovascular disease among the ageing population of Thailand. The 3G rice and well-designed meal plans received positive feedback from participants and can be used as a viable solution to prevent NCDs in Thailand’s ageing population.
A diet intervention was found to result in a more significant reduction in BW, BWI, VF, and HF among adult cohorts compared to a regular diet. However, exercise intervention had fewer effects on BMI, VF, and HF but no difference in BW compared to routine exercise. A range of meals were developed and served to the metabolic cohort during the intervention, including Thai Papaya Salad, Fried Fish Cakes, and Tom Yum Kung. The stools collected from MBC members were analysed for gut microbiota, leading to the identification of 90 microbial isolates from T2D and OB patients. The isolated gut microbiota from OB contained 53:42:5 for Gamma: Beta: Alpha hemolytic bacteria, while the isolated microbiota from T2D had 82:16:2 for Beta: Gamma: Alpha hemolytic bacteria. The National Research Council of Thailand (NRCT) has provided financial support for this ongoing project.
Don’t miss interesting posts on Famousbio